Mood Swings or Something More?
If you’ve been riding an emotional rollercoaster—feeling energized and unstoppable one week, then completely drained and hopeless the next—you might be wondering: Is this just depression, or could it be something else?
It’s a question many people ask themselves, often in the quiet moments when they’re trying to make sense of their shifting moods. The truth is, bipolar disorder and depression can look surprisingly similar on the surface, but understanding the differences is crucial for getting the right support and finding lasting stability.
At Focused Connections Psychiatry, we’ve walked alongside countless individuals who initially thought they were dealing with depression, only to discover that their mood patterns told a more complex story. Let’s explore what sets these conditions apart—and why that distinction matters for your journey toward feeling like yourself again.
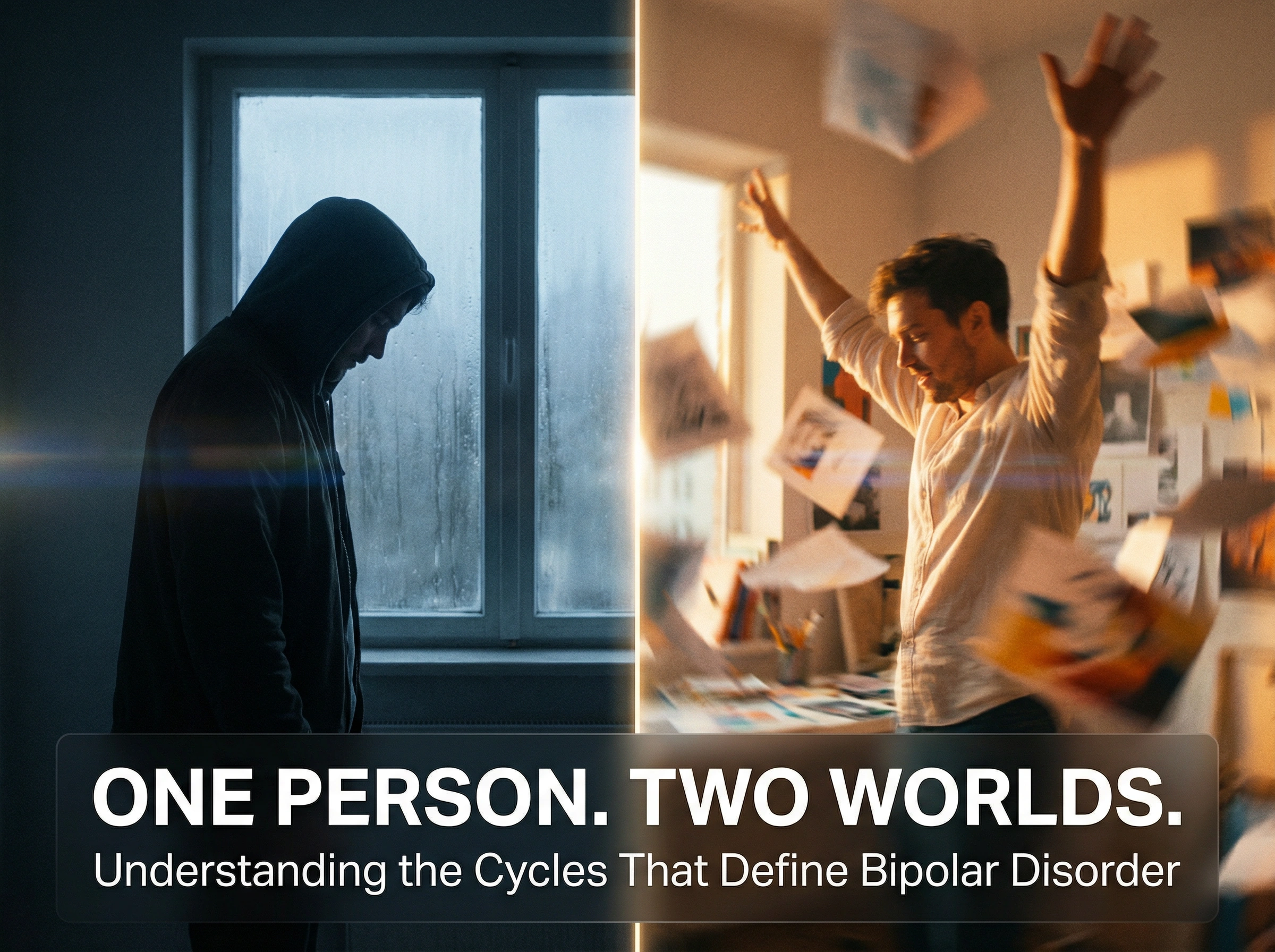
The Core Difference: It’s All About the Cycles
The most fundamental difference between bipolar disorder and major depression lies in the pattern of mood changes.
Major depression involves persistent low mood, loss of interest in activities, fatigue, and feelings of hopelessness that last for weeks or months at a time. It’s like being stuck in a fog that won’t lift—everything feels heavy, slow, and gray.

Bipolar disorder, on the other hand, involves distinct mood episodes that cycle between emotional extremes. People with bipolar experience periods of depression and periods of elevated mood—either full-blown mania (in Bipolar I) or hypomania (in Bipolar II). These “up” periods are what distinguish bipolar from depression alone.
Think of it this way: if depression is a valley you can’t seem to climb out of, bipolar is a landscape of both valleys and peaks—sometimes predictable, sometimes surprising, but always shifting.
What Do Those “Up” Periods Actually Look Like?
This is where things get interesting—and often confusing. Many people don’t realize they’re experiencing hypomania or mania because these states can feel good, at least initially.
During a manic episode (Bipolar I), you might:
- Feel unusually energetic or “wired,” even on very little sleep
- Talk rapidly, jumping from idea to idea
- Feel invincible or overly confident
- Take on multiple projects at once
- Make impulsive decisions—spending sprees, risky investments, sudden life changes
- Experience racing thoughts that won’t slow down
Hypomania (Bipolar II) is similar but less intense. You might feel incredibly productive, creative, and social. You’re sleeping less but don’t feel tired. Friends might comment that you seem “really on” or unusually upbeat. The key difference?
Hypomania doesn’t typically cause severe problems at work or require hospitalization, but it’s still a significant shift from your baseline.
Here’s the tricky part: these elevated periods often feel like relief after depression. “Finally, I’m back to normal!” you might think. But when the energy becomes excessive, sleep disappears, or decisions start having consequences you regret, it’s a sign that something more than a mood lift is happening.

The Depression Side of Bipolar
The depressive episodes in bipolar disorder can be indistinguishable from major depression. You might experience:
- Profound sadness or emptiness
- Loss of interest in things you once enjoyed
- Significant fatigue or low energy
- Difficulty concentrating or making decisions
- Changes in sleep (too much or too little)
- Feelings of worthlessness or hopelessness
What makes bipolar depression particularly challenging is that it often lasts longer and can be more treatment-resistant than the elevated episodes. Many people with bipolar spend far more time in depressive states than in manic or hypomanic ones.
Why the Distinction Matters for Treatment
Here’s why getting the right diagnosis is so important: the treatments for depression and bipolar disorder are different.
Standard antidepressants, when used alone in someone with undiagnosed bipolar disorder, can sometimes trigger manic or hypomanic episodes, or cause rapid cycling between mood states. This is why some people feel worse or more unstable after starting depression treatment—their underlying condition wasn’t fully understood.
Bipolar disorder typically requires mood stabilizers or other medications specifically designed to prevent both the highs and lows. Treatment is about creating stability—a steady emotional baseline where you can function, make sound decisions, and maintain healthy relationships.
“Could This Be Me?”
If you’re reading this and thinking, “Some of this sounds familiar,” you’re not alone. Many people with bipolar disorder go years—sometimes a decade or more—before receiving an accurate diagnosis. They might be treated for depression repeatedly without lasting improvement, or they might not recognize their elevated periods as symptoms at all.

Some questions to consider:
- Have you ever had periods where you felt unusually energetic, needed very little sleep, or took on way more than usual?
- Do your moods seem to cycle in patterns, rather than staying consistently low?
- Have antidepressants ever made you feel “wired,” agitated, or unusually activated?
- Has anyone close to you expressed concern about changes in your behavior or energy levels?
You Deserve Clarity and Support
Understanding whether you’re experiencing depression, bipolar disorder, or something else entirely isn’t about labels—it’s about getting care that actually works for your unique patterns.
At Focused Connections Psychiatry, we take the time to understand your complete mood history, including the highs, the lows, and everything in between. Through compassionate evaluation and collaborative conversation, we help you gain clarity about what’s happening and develop a treatment plan designed for lasting stability.
Your experiences deserve to be understood, not dismissed. If your moods feel like a puzzle you can’t quite solve, reaching out for a professional evaluation is a powerful step toward finally feeling like yourself again.
Ready to explore what’s really going on? Contact us at (562) 312-1777 today or click here to schedule your free symptom assessment. You’re not alone in this—and clarity is closer than you think.