Understanding the Overlap That Confuses So Many
You wake up exhausted even after eight hours of sleep. Your chest feels tight, your mind races with worry, yet somehow you also feel… numb. Empty. You can’t tell if you’re anxious about everything or just don’t care anymore.
When you finally Google your symptoms at 2 AM, you’re left more confused than before. Is this anxiety? Depression? Am I dealing with both?
If this sounds familiar, you’re not alone. At Focused Connections Psychiatry, we see this confusion every single day—and for good reason. Anxiety and depression aren’t just common companions; they’re so intertwined that distinguishing between them can feel impossible without professional guidance.
Why the Lines Get Blurry
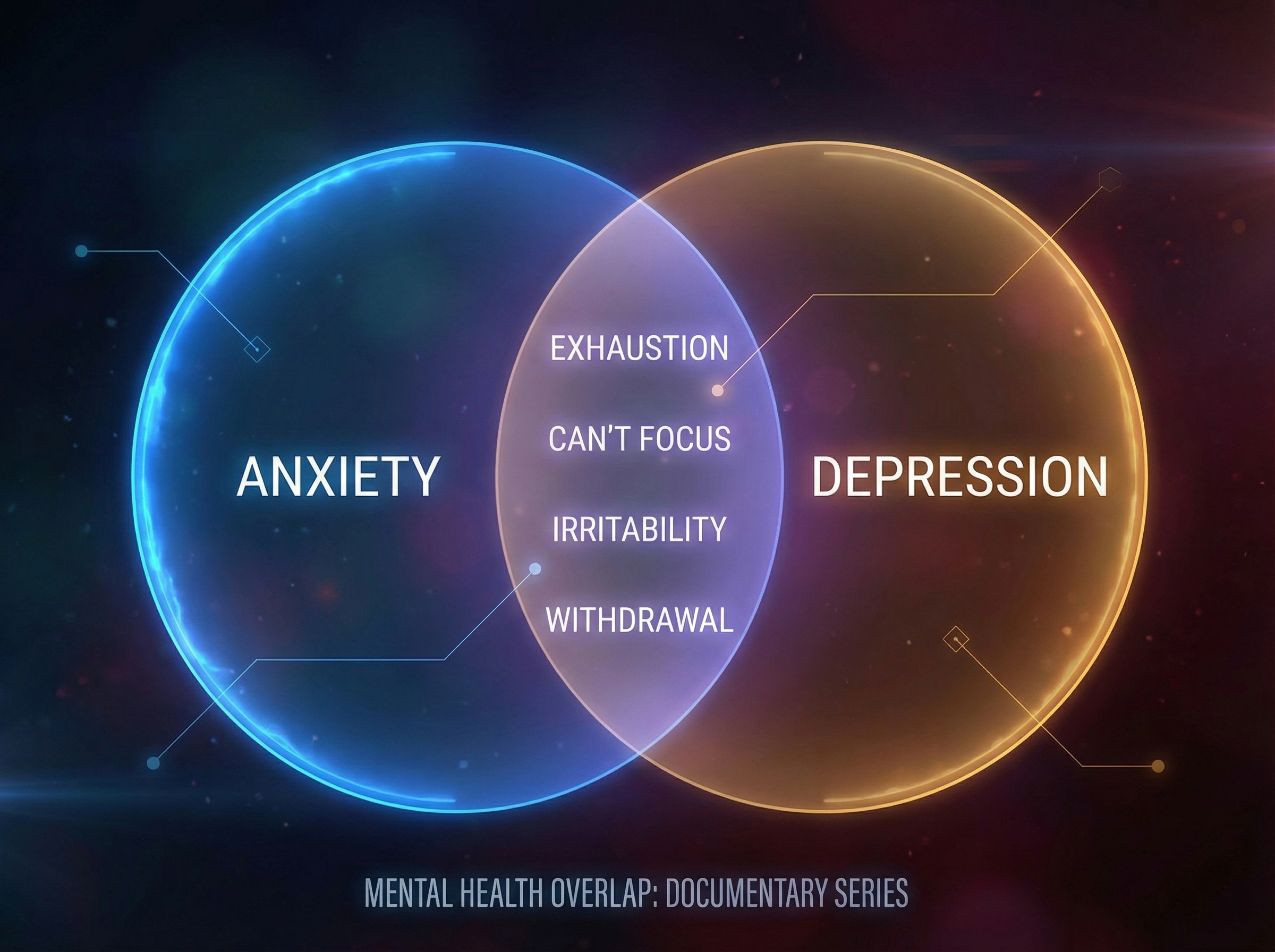
Here’s what makes this so confusing: anxiety and depression share a surprising amount of common ground. Both can cause:
- Difficulty sleeping (though for different reasons)
- Trouble concentrating and brain fog
- Physical exhaustion that rest doesn’t fix
- Irritability that seems to come out of nowhere
- Withdrawal from activities and people you once enjoyed
- Physical symptoms like headaches, muscle tension, and digestive issues
When you’re experiencing several of these symptoms simultaneously, your brain isn’t trying to trick you—it’s genuinely hard to tell what’s driving what.
Is the exhaustion from anxiety keeping you up at night, or is it the heavy fatigue of depression? Are you avoiding social situations because of anxious fear or depressive apathy?
The Key Differences (When You Look Closer)
While overlap is common, anxiety and depression do have distinct emotional signatures:
Anxiety tends to be future-focused. It’s the “what if” spiral—constant worry about things that might go wrong, fear of losing control, and a persistent sense that danger is lurking around every corner. Your body stays in high alert mode: racing heart, chest tightness, restlessness, and that feeling of being perpetually “on edge.” You’re often moving fast mentally and physically, even when exhausted.
Depression, on the other hand, often feels like being stuck in quicksand. It’s less about racing thoughts and more about heavy, persistent sadness or emotional numbness. The future doesn’t spark worry—it just feels hopeless or pointless. You might struggle to find joy in anything, feel guilty without a clear reason, or have thoughts that you’re a burden to others. Where anxiety speeds you up, depression slows you down.
But here’s the complicating factor: you can absolutely have both at the same time.
When Anxiety and Depression Show Up Together
Research shows that nearly 60% of people with depression also experience significant anxiety symptoms, and about half of those with anxiety disorders also struggle with depression. This isn’t a coincidence—these conditions share similar brain chemistry imbalances and often feed into each other.
Here’s how the cycle typically works:
Chronic anxiety is exhausting. When your nervous system stays in overdrive for weeks or months, it depletes your emotional reserves. You start avoiding more situations, isolating yourself, and feeling hopeless about ever feeling calm again. That’s when depression can creep in.
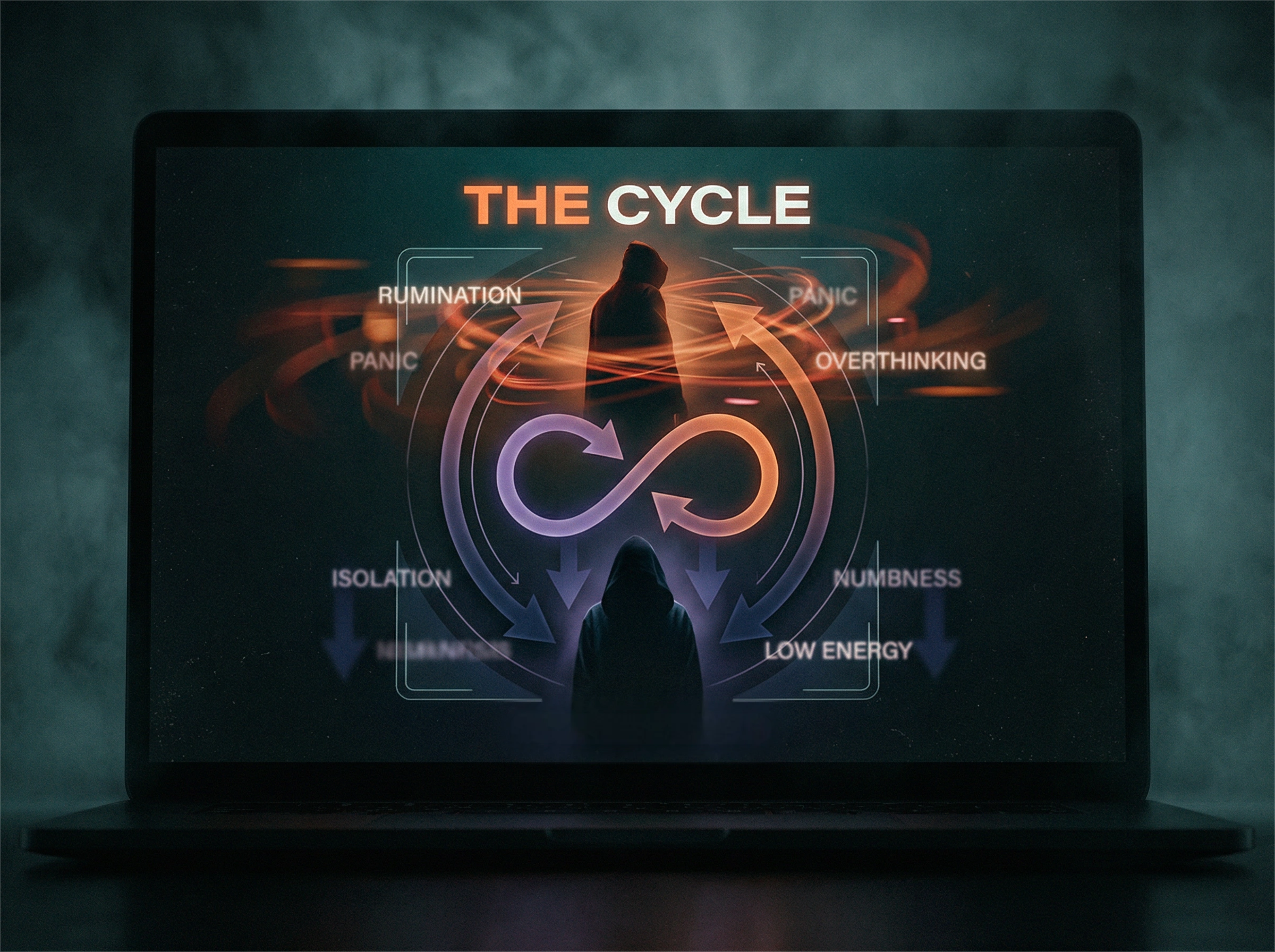
Conversely, depression can trigger anxiety. When you’re already feeling low and struggling with daily tasks, you might start worrying intensely about your inability to function, your relationships falling apart, or your future looking bleak. The worry compounds the depression.
This overlap is why self-diagnosis rarely works and why professional evaluation is so important.
What This Means for Your Treatment
Understanding whether you’re dealing with anxiety, depression, or both isn’t just about labels—it directly impacts your treatment plan and your path to feeling better.
Different conditions respond to different approaches. Some medications work well for anxiety but may not fully address depression, and vice versa.
Therapy techniques that help with anxious thought patterns differ from those that target depressive thinking. When both conditions are present, your treatment needs to address both—and that requires a clear, comprehensive evaluation.
At Focused Connections Psychiatry, we don’t rush to conclusions. During your evaluation, we take time to understand:
- When your symptoms started and how they’ve evolved
- What your symptoms feel like in your body and mind
- How your symptoms affect your daily life, relationships, and work
- Your personal and family mental health history
- What makes your symptoms better or worse
This thorough approach helps us see the full picture—not just surface symptoms, but the underlying patterns driving your distress.
You Don’t Have to Figure This Out Alone
If you’re reading this and thinking, “This is exactly what I’m going through,” please hear this: the confusion you feel is valid, and you don’t need to have it all figured out before reaching out.
You don’t need to know whether it’s anxiety, depression, or both. You don’t need to determine if your symptoms are “serious enough.” If what you’re experiencing is affecting your daily life, your relationships, or your sense of self—it’s worth discussing with a professional.
Many people find that simply having someone help them understand what’s happening brings immediate relief. When you can finally put words to your experience and know there’s a path forward, the weight starts to lift.
At Focused Connections Psychiatry, we combine compassionate, individualized care with evidence-based evaluation to ensure every diagnosis and treatment plan brings you closer to lasting clarity and emotional balance. Because you deserve care that truly understands you—in all your complexity.
Ready to get clarity? Contact us at (562) 312-1777 today or click here to schedule your free symptom assessment. Your journey toward understanding and relief starts here.